
Osteochondrosis of the cervical spine (SC) is one of the most common pathologies of the musculoskeletal system. Every year doctors diagnose this disease more and more frequently, and its course becomes more severe. According to statistics, in women, degenerative-dystrophic changes in the upper spine occur more often, especially in patients in the postmenopausal period. The main symptoms of cervical osteochondrosis in women are pain, limited mobility and cerebrovascular insufficiency, and this is dangerous not only for health but also for life. To protect yourself from the dangerous consequences of pathology, you should start its treatment in the early stages. It is important to carry out complex therapy and change lifestyle to stop the destruction of spinal segments and prevent serious complications.
Development of the disease.
The cervical spine is most vulnerable to various injuries and degenerative changes. This is due to the fact that this segment is the most mobile and the muscles here are weak. Small cervical vertebrae endure heavy loads every day, which leads to the gradual destruction of the intervertebral discs. The vertebrae press against each other, causing the cartilage pads between them to lose a lot of fluid and begin to degrade and deform.
Also, osteochondrosis of the cervical spine develops due to insufficient nutrition of the cartilaginous tissue. And the spinal canal in this area is narrow, so it often becomes compressed, causing neurological symptoms.
Pathology in women in the early stages is manifested by heaviness in the back of the head, tingling in the hands, etc. Patients often mistake the first signs of the disease for fatigue.
In the neck area there are a large number of blood vessels and nerve roots; when they are compressed, neurological disorders can also occur. It is especially dangerous if a deformed disc or vertebra compresses the vertebral artery, which supplies important parts of the brain. When it is compressed, the coordination of movements is affected, the woman may lose balance, her vision and hearing deteriorate, and the risk of suffering a stroke increases.
Reference.According to statistics, cervical osteochondrosis is most often found in patients between 25 and 40 years old. This is due to a massive decrease in physical activity and sedentary work. Women are diagnosed with the disease more often than men, as they have more fragile vertebrae and thin bone tissue.
Doctors distinguish 4 stages of osteochondrosis of the spine:
- Level 1– the intervertebral disc loses part of its moisture, its height decreases and cracks may appear in the annulus fibrosus (outer layer). This is the stage of cervical chondrosis, which is difficult to identify, since it has unexpressed symptoms. The neck gets tired quickly, there is discomfort, heaviness in the damaged area, sometimes there is a slight pain that passes quickly.
- Stage 2– cracks on the surface of the disc increase, the nucleus pulposus (the gelatinous contents of the disc) shifts and may protrude through the damaged areas. This is how protrusions of the cartilage lining appear, which can compress the spinal cord and its roots. Severe pain, weakness, limited mobility, and numbness of the face, neck, shoulders, and arms may occur periodically.
- Stage 3– the bulge pierces the outer layer of the disc, thus forming a hernia. The pain becomes more pronounced and neurological disorders occur.
- Stage 4– the disc is almost completely destroyed, the vertebrae rub against each other and bone growths (osteophytes) appear on their edges, which are designed to stabilize the damaged segment. Nerve endings, spinal cord and blood vessels are infringed. Adjacent joints begin to become damaged. Clinical signs are pronounced.
The easiest way to stop degenerative-dystrophic changes is in the first two stages of osteochondrosis of the spine. In stage 3, comprehensive treatment will help stop further destruction of the spinal segment. In the last stage, surgery cannot be avoided.
Causes
Osteochondrosis of the spine is a complex and prolonged process that usually has several causes. In most cases, pathology occurs due to a sedentary lifestyle, poor nutrition and metabolic disorders. The disease is often caused by an injury or by the natural aging of the body and the weakening of its defenses.
Doctors identify the main causes of osteochondrosis of the spine in women:
- Violation of metabolic processes.
- Passive lifestyle.
- Genetic predisposition.
- Chronic muscle tension around the cervical segment.
- Posture distortion.
- Deficiency of fluids and nutrients in the body.
- Prolonged stay in an uncomfortable position (neck stretched forward and back hunched).
- Excessive weight.
- Frequent use of high-heeled shoes.
- SHOP injuries.
- Lift heavy objects.
- Autoimmune pathologies.
- Frequent stress, chronic fatigue.
- Hypothermia.
- Infectious diseases.
- Neck too long or short, etc.
All these factors cause malnutrition of the intervertebral discs and lead to their degeneration.
Female cervical osteochondrosis can be caused by pathologies of the vertebral artery associated with genetic predisposition, intrauterine disorders and injuries during childbirth. The disease can occur due to rheumatism, endocrine disorders, excessive load on the cervical segment during pregnancy and local overload.
Important.The main cause of cervical osteochondrosis in women is menopause, as well as the changes associated with this period. At this stage, the concentration of progesterone in the body decreases, which is very important for bone tissue. The likelihood of degenerative changes is associated with age-related weakening of the neck muscles and weakening of spinal support in this area.
Symptoms
Osteochondrosis is characterized by an undulatory course, when the acute period gives way to remission. Exacerbation can be caused by infections, injuries, hypothermia, and prolonged tension in the neck.

The first signs of cervical osteochondrosis in women are headaches, discomfort and heaviness in the neck. It is important to distinguish pain due to chondrosis from migraine or autonomic dysfunction in time.
Clinical manifestations of osteochondrosis of the spine in women are caused by neurological syndromes:
- Cervical dyscalgia occurs when nerve endings are irritated by fragments of damaged cartilage lining. Then a specific crackling appears in the neck, pain that becomes more pronounced when moving the head and after sleeping.
- Scalenus syndrome is a consequence of damage to the vessels and nerves of the brachial plexus and subclavian artery. This symptom complex is accompanied by pain from the inner surface of the shoulder to the hand on the injured side. The limb becomes pale, cold, swollen and numbness occurs. Neck pain extends to the back of the head when the patient turns his or her head.
- Humeral periarthrosis syndrome: dystrophic changes affect the tendon fibers surrounding the shoulder. Painful sensations from the neck radiate to the shoulders and shoulder girdle. There is a forced position of the neck: it is tilted to the affected side, and the shoulder is slightly lowered.
- Vertebral artery syndrome: A blood vessel is compressed by fragments of a damaged disc or osteophytes (depending on the stage of the disease). The patient feels dizzy and has headache, nausea, and sometimes vomiting. The pain is located in the neck, crown and temples.
- Cardiac: the nerve bundles of the spinal cord are damaged. Heart pain and arrhythmia occur. If C3 is damaged, pain appears in the middle of the neck, the tongue swells, and the patient cannot chew food normally. If C4 is injured, discomfort appears in the area of the shoulder girdle, clavicle and heart. When C5 is affected, the neck pain reaction extends to the shoulder girdle, the inner surface of the shoulder. C6 irritation causes pain from the neck and shoulder blade to the shoulder girdle and extends down the entire arm to the thumb. If C7 is damaged, the pain syndrome extends to the back of the shoulder girdle and affects the entire hand, including the index and middle fingers. When C8 is compressed, the pain extends from the affected area to the elbow and little finger.
In addition, a woman's emotional sphere may be disturbed, weakness may appear, she becomes anxious and touchy. Insomnia often occurs, memory and attention are weakened due to regular headaches.
Stroke symptoms occur when a woman suddenly throws her head back, tilts her head, or does work that puts pressure on her arms and cervical spine, for example, when she digs, paints a roof, or carries heavy objects.
Poor cerebral circulation is manifested by dizziness, unsteady gait, spots before the eyes, tinnitus, weakness and nausea. In some patients, the voice becomes hoarse, sometimes disappears, and a sore throat appears.
Osteochondrosis during menopause is accompanied by migraines, increased body sweating in the area between the neck and shoulder girdle. When the vertebral artery is compressed, the functioning of the cardiovascular system is impaired.
If the disease lasts a long time, circulatory failure occurs in important centers that perform neuroendocrine functions. Due to increased permeability of vascular walls, atherosclerosis of the cerebral and cardiac arteries develops.
Establish diagnosis
If you notice symptoms of osteochondrosis, see a therapist. After a visual examination, the specialist will refer you to an orthopedist, vertebrologist or neurologist.
The following methods are used to diagnose cervical osteochondrosis:
- The x-ray allows us to know that the patient's vertebrae are displaced, there are osteophytes on their edges, the distance between the vertebrae has decreased, etc. For this, the study is carried out on different levels. To detail the characteristic changes, the doctor takes specific photographs.
- Computed tomography of the cervical spine provides detailed information about pathological changes in the vertebrae. This method allows obtaining three-dimensional images for a more detailed study; it is used in cases of severe diagnosis.
- MRI is used to accurately assess the condition of soft tissues (nerves, blood vessels, ligaments, muscles) in the affected area.
- Electromyography allows you to check the conductivity of the nerve fiber.
Doctors may also prescribe an ultrasound (Doppler ultrasound of the main arteries of the brain) to determine the status of blood flow in this area.
Conservative treatment
In the early stages, treatment of osteochondrosis of the spine in women can be done at home. However, a doctor must develop a treatment regimen. It is important to understand that this is a long process and a full recovery is unlikely to be possible (especially for older women).
Complex treatment includes:
- Taking medicines.
- Use of orthopedic devices.
- Physiotherapy.
- Physiotherapeutic procedures.
- Massage, manual influence.
- Alternative treatments.
Conservative methods will help relieve pain, inflammation, normalize muscle tone, improve metabolic processes, nourish damaged segments of the spine, etc. With timely therapy, it is possible to stop pathological changes.

Treatment of cervical osteochondrosis in women is carried out with the use of medications that will help improve the metabolism of the cartilage pads between the vertebrae and relieve inflammation and pain. For this purpose, the following medications are used:
- NSAIDs. They will help relieve inflammation and pain of mild or moderate severity.
- Analgesics. Alleviate the pain.
- Medications to improve cerebral circulation.
- Muscle relaxants help relieve muscle spasms.
- Chondroprotectors. They help stop disc destruction, improve metabolic processes and speed up recovery.
- Magnesium-based medications.
- Nootropics. They stimulate the functioning of the brain, normalizing its blood circulation and have a mild sedative effect.
Reference.For severe pain that is not relieved by oral medications, therapeutic blocks are used, for example with an anesthetic solution or NSAID.
The treatment can be complemented with anti-inflammatories and analgesics in the form of gels, creams and ointments. They will be effective in the remission stage or in combination with oral medications.
The decision on the choice of drug combinations is made by the doctor. The specialist will draw up a medication regimen and also determine its dosage. It is important to follow their recommendations, since many of the medications described above can lead to dangerous complications.
During the acute stage of osteochondrosis of the spine, a woman should abandon intense physical activity. To relieve the cervical segment, it is necessary to use a special corset (Schants collar), which will fix the vertebrae in the correct position. The use of this device is recommended during prolonged, sedentary or intense physical work.
Physiotherapeutic procedures will help relieve pain and improve blood circulation in the damaged area:
- Diadynamic therapy.
- Magnetotherapy.
- Electrophoresis with an anesthetic, glucocorticosteroid, proteolytic agent.
- Electroanalgesia.
- Ultraviolet irradiation, etc.
The therapeutic effect appears approximately after the third session, then headaches, hearing and vision disorders, dizziness attenuate or disappear, sleep normalizes and the general condition improves.
Using underwater traction of the cervical segment, you can expand the distance between the vertebrae, free a nerve or blood vessel from compression, and restore the normal position of the vertebrae.
Massage will normalize muscle tone and reduce the flow of lymphatic fluid, which causes swelling. After several sessions, blood circulation in the damaged area improves.
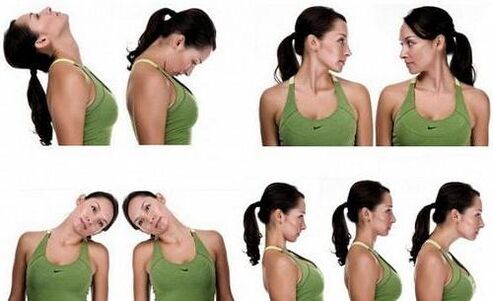
Therapeutic gymnastics is one of the most effective methods of treating osteochondrosis of the spine. Exercise therapy allows you to strengthen weak neck muscles, which will then absorb some of the load from the spine and help stop or slow down degenerative changes. During exercise, blood circulation improves, metabolic processes and nutrition of the disc are accelerated, which has a positive effect on its condition.
Women should exercise every day. They consist of simple but effective exercises. The complex consists of turns, tilts of the head in different directions, as well as movements of the neck, during which the arms are used. These items can be performed at home, but only with a doctor's permission. Physiotherapy is carried out only in the remission stage.
Complex treatment can be complemented by reflexology (acupuncture), hirudotherapy (treatment with leeches), swimming, etc.
Surgery
The operation is prescribed in the late stages of osteochondrosis of the spinal cord, which are accompanied by severe destruction of osteochondral structures. In addition, surgical intervention cannot be avoided if conservative methods are ineffective or the spinal canal has narrowed significantly.
In the above cases, an anterior cervical discectomy is performed. During the procedure, the doctor immobilizes the damaged segment of the spine and removes the hernia that was compressing the spinal nerve. The vertebrae between which the disc was removed are then fused. If necessary, the space between the vertebrae is filled with a synthetic insert (cage).
After 3 to 5 days, the patient is discharged. The rehabilitation period is about 12 weeks. To speed up recovery, you need to take medication, wear a corset, lead a healthy lifestyle, go to physiotherapy procedures and, finally, do exercise therapy.
Lifestyle recommendations
To quickly get rid of the unpleasant symptoms of osteochondrosis and stop degenerative-dystrophic changes in the cervical segment, you need to adjust your lifestyle. To do this, the patient must follow these recommendations:
- Go for a walk every day, avoid running, jumping and other explosive activities.
- Do not carry heavy objects.
- You cannot sit for a long time, in extreme cases, wear a corset and periodically take a horizontal position.
- Do special physical exercises for the back muscles at home.
- Sleep on an orthopedic mattress and a special pillow.
- Follow a diet, replenish your diet with foods rich in magnesium, calcium (nuts, dairy products, seafood, legumes), as well as plant fiber, chondroitin (jellied meat, gelatin). Avoid fatty, fried, overly salty foods and alcohol. Your doctor will advise you in more detail about nutritional standards. But in any case it must be correct.
Hypothermia should not be allowed, warming will be beneficial in the absence of an inflammatory process.
Complications
In the absence of timely treatment of cervical osteochondrosis, a woman may experience the following consequences of pathology:
- The likelihood of a bulge, which after a while transforms into a hernia. The lump compresses the spinal cord and its nerves, causing neurological disorders.
- Osteophytes appear when the disc is severely damaged and irritate the spinal nerves and blood vessels.
- In advanced cases, severe weakening of the neck muscles or incomplete paralysis is possible, then the head hangs involuntarily to the side or forward.
- Compression of the vertebral arteries, alteration of circulation in the affected area. This condition can cause neuralgia (pain along the nerve), hearing and vision problems.
- Paralysis (incomplete or complete) of the hands.
- Stroke, etc.
If a woman addresses the problem in the early stages of osteochondrosis of the spinal cord, she will be able to prevent the conditions described above.
Precautionary measures
Ideally, prevention of osteochondrosis of the spine should be carried out during the period of intrauterine development. The future mother must exclude factors that negatively affect the development of the fetus: infections, lack of oxygen, intoxication. If there has been a birth injury, the newborn must undergo treatment.
To reduce the likelihood of developing osteochondrosis of the spine, a woman should follow these recommendations:
- Load her spine evenly, for example, carry a load with both hands or alternately with the right and then the left.
- Don't lift too much weight on your own.
- Try to avoid neck injuries and hypothermia.
- While working on garden plots, take a break every 1. 5 hours and lie down to rest for 20 minutes.
- Choose shoes with elastic soles that cushion impacts when running or jumping.
- When sitting for long periods of time, use a high-back chair with a headrest or wear a corset.
It is also important to eat well, control weight, avoid stress, take vitamin supplements for medical reasons and quickly treat pathologies that can cause osteochondrosis. During the remission stage, it is recommended to visit sanatoriums to undergo treatment.
The most important
As you can see, osteochondrosis of the cervical spine occurs more often in women than in men, since the former have more fragile vertebrae and thin bone tissue. Patients during the postmenopausal period are especially susceptible to pathology. The disease is manifested by pain, neurological disorders and dangerous symptoms of stroke. It is recommended to start treatment in the early stages to avoid dangerous complications of osteochondrosis. To do this, the woman must take medications, adjust her lifestyle, attend physiotherapeutic procedures, massages, perform physical therapy, etc. Surgical treatment is indicated only in advanced cases. To prevent pathology, it is necessary to maintain moderate physical activity, quickly treat injuries and diseases that can cause osteochondrosis, etc.

























